In the quiet, highly technical world of cancer imaging, a new line of research is offering something patients and doctors have long hoped for: clearer answers at one of the most uncertain moments in prostate-cancer care. When cancer appears to return after surgery, physicians often have to make treatment decisions with limited information. A new study suggests that a modern imaging technique may change that equation.
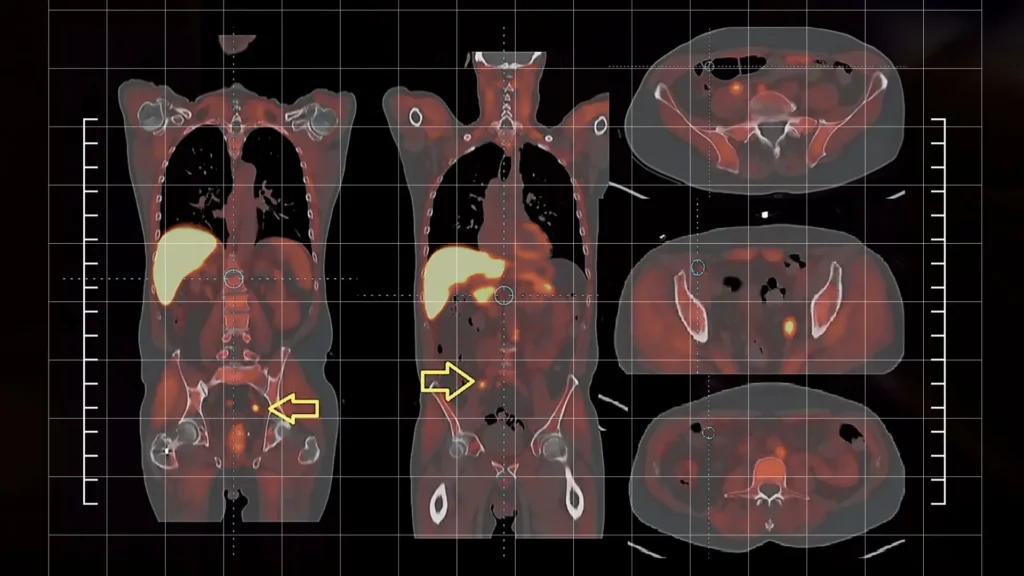
The research focuses on a scan known as PSMA PET/CT, a technology that has been steadily gaining attention in oncology clinics. Unlike older imaging methods that sometimes struggle to detect tiny cancer deposits, PSMA PET/CT uses a tracer that binds to a protein commonly found on prostate-cancer cells. The result is a scan that can reveal cancer activity at much earlier stages and in much smaller amounts.
In the new study, published in the February 2026 issue of a major oncology journal, researchers analyzed data from 113 men treated for prostate cancer at UCLA’s Jonsson Comprehensive Cancer Center. All of the patients had undergone surgery and later showed signs of biochemical recurrence, meaning their prostate-specific antigen, or PSA, levels had begun to rise again.
That rising PSA is often the first warning sign that the cancer may be returning, but it does not reveal where the disease is located. For decades, doctors have had to rely on less sensitive imaging or make treatment decisions based on educated guesses. The PSMA PET/CT scans changed that picture.
The study divided patients into groups based on what the scans revealed. Some showed no visible disease at all. Others had localized recurrence, and a third group had cancer that had already spread to lymph nodes or distant sites. Those distinctions turned out to matter.
Patients whose scans showed no visible disease had the most favorable progression-free survival. In those cases, expanding radiation to the whole pelvis offered no significant benefit over more targeted radiation to the prostate bed alone.
But the story was different for patients whose scans revealed localized recurrence. For them, whole-pelvis radiotherapy significantly improved outcomes, suggesting that broader treatment made sense when the disease was actually visible in that region.
And for patients whose scans showed cancer in lymph nodes or distant sites, the addition of androgen-deprivation therapy, a hormone-blocking treatment, was associated with better progression-free survival. In other words, the scan was not just detecting cancer. It was helping guide the next move.
Lead researcher Dr. John Nikitas emphasized the practical implication of the findings, noting that the study highlights the importance of using PSMA PET/CT scans routinely for patients with biochemical recurrence after prostate-removal surgery.
For patients, recurrence after prostate surgery can be an emotionally fraught time. PSA levels rise, but the location of the disease is uncertain. Doctors must decide whether to use radiation, hormone therapy, or a combination of treatments, often without precise imaging guidance.
This is where PSMA PET/CT may mark a turning point. Instead of treating all patients with a one-size-fits-all approach, the new data suggest that therapy can be tailored to what the scan actually shows. If no disease is visible, treatment can be more conservative. If the cancer is localized, radiation fields can be expanded. And if it has spread, systemic therapy can be added earlier.
That level of personalization is increasingly becoming the goal across oncology, but it depends heavily on imaging that can detect cancer at its earliest stages.

Sana A. is a medical student, writer, and journalist with a strong passion for healthcare reporting and a deep commitment to covering current events across the United States. As a contributor to Los Angeles Headlines, she focuses specifically on medical news, health policy, and emerging trends in the healthcare industry.